Children’s Breathing Problems Treatment
Are you worried that your child may be experiencing behavioral problems, fatigue, or slow growth? It’s often a source of worry for many parents that their children aren’t acting or developing as they should, but there might be a fairly simple explanation for these problems: Your child might not be getting adequate sleep.
This lack of shut-eye may be due to something called sleep-disordered breathing, and the good news is there are many treatments for this condition.
What is Sleep Disordered Breathing?
Sleep-disordered breathing or SDB, is a broad term used to describe problems that arise during sleep. Two common examples of SDB are upper airway resistance syndrome (UARS) and obstructive sleep apnea (OSA). Snoring can affect about 10% of children, and 2-4% experience obstructive sleep apnea, where part or all of the airway is blocked at various points during sleep. OSA prevalence may be closer to 5% however, due to the obesity epidemic among children today. The greatest incidence of OSA occurs between the ages of 2 and 8. Prevalence of UARS in children is unclear due to debate as to how to measure disordered breathing “events”.
These events can routinely interrupt your child’s sleep, leading to a wide variety of other problems during waking hours.
While everyone needs a good night’s sleep, it’s particularly important for children to be rested, as they are going through immense periods of physical and neurological growth. Children 4-12 years old need 10 hours of sleep per night. Sleep deprivation in children can lead to emotional problems like irritability and hyperactivity.
It can also affect children in myriad other ways:
-
- Learning difficulties: Because of sleep deprivation, your child may exhibit behaviors like moodiness and disruptiveness, even contributing to the development of attention deficit disorder (ADHD). Additionally, children who snore during childhood are at greater risk of poor academic performance in later years.
-
- Obesity: Due to SDB, children have the dual factors of decreased daytime activity due to fatigue, as well as increased resistance to insulin. Release of hormones like ghrelin and leptin, which affect children’s ability to regulate weight, are disrupted during poor sleep. This combination can put a child more at risk for obesity and related health problems like diabetes.
-
-
- Slower growth and development: Since the brain produces a good amount of growth hormone (GH) at night when your child is sleeping, an interruption in this process can cause underdevelopment due to a lower level of GH. Long-term, this can slow your child’s growth and development, yet is avoidable.
- Pulmonary and cardiovascular disorders: Constantly waking up throughout the night increases both your child’s heart rate and blood pressure, both of which add stress to the body’s vascular system. The body responds to stress by producing a hormone called cortisol, which also causes wear and tear on the body’s vasculature over time. Additionally, a lower level of oxygen throughout the night can lead to both respiratory and cardiac problems in the long term, as the body struggles to compensate for the physiologic chaos.
-
How Your Dentist Can Detect Sleep Disordered Breathing in Children
Oral care is important to everyone’s well-being, so it’s crucial to develop good habits when children are still young. This is particularly important when it comes to checking your child’s airway and seeing if there is any potential that she might have sleep-disordered breathing. Your dentist can help by performing a thorough oral assessment at every teeth cleaning appointment.
Predisposing factors, signs, and symptoms of SDB that your dentist might note, include:
-
- Race and gestational maturity: African American and preterm infants have higher rates of SDB than their white or full-term counterparts.
-
- Bedwetting: Also known as nocturnal enuresis, this is a common sign of disturbed sleep.
-
- Breathing patterns: Let your dentist know if your child typically breathes loudly, or is a mouth breather when they sleep. These are clues that SDB might be present.
-
-
- Sleep disturbances: Restless sleep, nightmares, and night terrors can all indicate potential SBD in your child.
- Frequent physical problems: Constant headaches, earaches, and upper airway infections can predispose your child to SDB.
-
-
- Behavior: ADD (Attention Deficit Disorder), ADHD (Attention Deficit Hyperactivity Disorder), moodiness, irritability, and hyperactivity can all be signs that your child is not sleeping well through the night.
-
-
- Obesity: Obesity can be both a cause and result of SDB, so your dentist will take note of your child’s body mass index (BMI) to determine if there might be an overlooked problem.
- Anatomy: Your child’s own bodily structures may make it difficult for him to breathe at night.
-
Adenotonsillar hypertrophy, or overgrowth of the adenoids and tonsils, may predispose your child to SDB. Much craniofacial anatomy is genetic; if anyone in your family suffers from SDB, chances are the children in your family will as well.
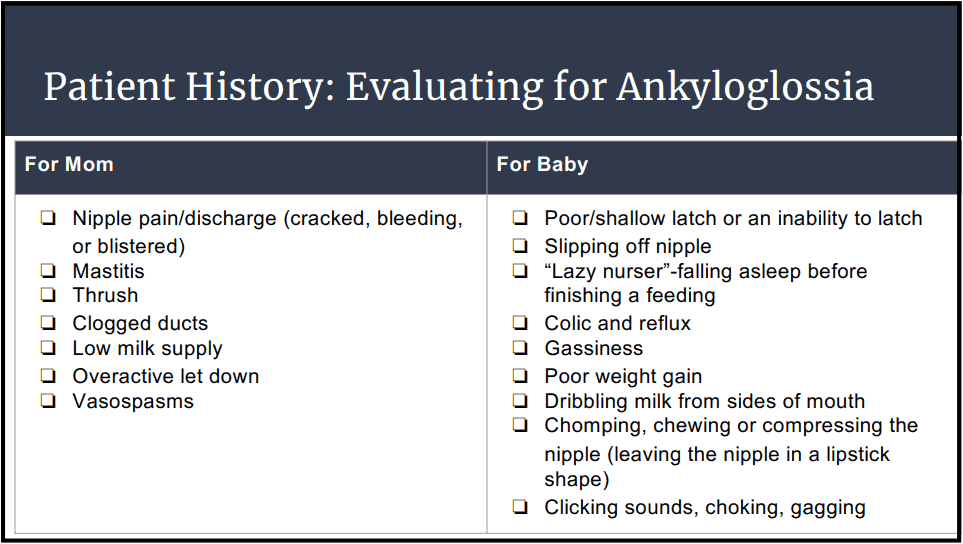
Ankyloglossia or “tongue-tie,” is a congenital oral anomaly where the lingual frenulum (the thin membrane connecting the tongue to the floor of the mouth) is too short for normal tongue movement. This can result in speech and breathing problems, particularly in children.
Compromised facial/jaw growth can be a cause of SDB. How the face and jaws grow is only partly influenced by genetics. Lack of correct breathing, swallowing, and tongue posture will cause disruption of growth in craniofacial structures which will even affect how your child’s teeth come in, or how they hold their head.
- Environmental exposure: Toxins like cigarette smoke are particularly hazardous to the sensitive airways of children and can result in problems like OSA and asthma.
- Genetic variation: Children with trisomy 21 (Down Syndrome) and cystic fibrosis (CF) are much higher at risk for SDB than those without these genetic inheritances.
Source: Wisconsin Sleep Society
Children and OSA
Delayed treatment of pediatric obstructive sleep apnea can lead to a persistent decline in cognitive function, leading to a potential decline in academic performance. While long-term effects are not completely known, there is evidence that the damage may not be reversible; that is, whatever problems your child has faced until diagnosis and treatment, may not fully resolve over time.
Diagnosing Sleep Disordered Breathing in Children
You and your dentist both suspect your child has SDB. Now what? There are typically a few steps that come next in order to get a medical diagnosis of pediatric sleep-disordered breathing.
- Get a referral. An otolaryngologist (also called an ENT or ear, nose, and throat doctor) can examine your child and can make a diagnosis based on the exam and the child’s history; otherwise, further testing may be warranted.
- Have a sleep study done. Polysomnography (PSG), better known as a sleep study, may be done to confirm a diagnosis of SDB. During this test, wires are painlessly attached to your child to measure muscular movements, brain waves, eye movement, breathing, and oxygenation during sleep. Please note that a PSG may be done before any surgical removal of the tonsils and/or adenoids. It is important to note that 80% of men and 90% of women with SDB go undiagnosed. What’s alarming is that even higher percentages of children are going undiagnosed. This is in part because of the definitions used by sleep medicine to determine whether an adult has SDB do not apply to children. Rarely is a child apneic. but rather they have arousals due to partial restriction of the airway, known as UARS, or upper airway resistance syndrome. The other reason kids aren’t being diagnosed is that pediatricians, pediatric dentists, and restorative dentists don’t recognize what they are seeing when examining these patients.
10 Signs Your Child May Suffer from Sleep Disturbance
If you’re concerned your child might be experiencing SDB, here are ten questions to ask yourself, then discuss with your dentist and other healthcare providers:
1. Does your child have trouble going to bed or falling asleep?
2. Does s/he awaken during the night and have trouble returning to sleep?
3. Does s/he tend to breathe through their mouth during the day or during sleep?
4. Does s/he have a dry mouth or bad breath upon waking in the morning?
5. Have you noticed any of the following while your child is sleeping?
- Snoring, heavy or loud breathing?
- A break or pause in breathing?
- Gasping, choking, or struggling to breathe?
- Restless or agitated sleep? Grinding teeth?
- Abnormal head posture (hyperextension, etc.)
- Excessive sweating?
- Wetting the bed?
6. Have you noticed any of the following during the day?
- Difficulty waking?
- Waking with headaches?
- Feeling groggy, tired or “out of it”?
- Hyperactivity?
- Teachers commenting on behaviors?
7. Does your child often:
- Not seem to listen when spoken to directly?
- Have difficulty organizing tasks?
- Get easily distracted by extraneous stimuli?
- Fidget with hands or feet or squirm in his/her seat?
- Interrupt or intrude on others?
8. Is your child frequently sick or have a history of sore throat, ear infections, sinus infections, or allergies?
9. Did your child stop growing at a normal rate at any time since birth? Is s/he overweight?
10. Does your child have habits such as: using a pacifier/ thumb sucking/ lip biting/ teeth grinding?
Treatments for Sleep Disordered Breathing in Children
If you find out your child does, in fact, have SDB, there is good news: This is a relatively common condition, and there are many treatment options available. From non-invasive dental appliances to full-on surgical removal of airway-obstructing anatomy, there is a wide spectrum for you and your healthcare professionals to choose from. Treatments should move from least to most invasive, and may include any or all of the following:
-
- Treating the underlying cause(s): If your child’s SDB is due to a factor like obesity, a weight-loss plan will help with relieving some of the symptoms. Asthma and diabetes can also be effectively managed to prevent further complications with SDB.
-
- Myofunctional therapy: Myofunctional therapists are like physical therapists for the tongue and airway. They help people to use muscles of their face and mouth to breathe, chew and swallow in a functionally correct and healthy way. Myofunctional therapy is often used in conjunction with dentists and other healthcare professionals to ensure your child resolves his/her problems through behavioral changes. They can also impact speech pathologies.
-
- Eliminating oral (mouth) breathing: If your child constantly snores and sleeps with his/her mouth open, nasal breathing should be encouraged while awake. At night, a simple intervention like mouth taping and wearing nasal dilators might work. Consult with your dentist to see if this could be an option for you and your child to try.
-
-
- Orthodontics: Studies show that a too-small upper jaw (maxilla) is one of the primary reasons for SDB in both adults and children. By expanding the palate with appliances and broadening the dental arches with braces, tongue space is created that will allow for nasal breathing, which in turn will help direct the skeletal growth of the jaws and increase the size of the airway. Bringing the lower jaw forward with functional orthodontics can help “grow” the jaw forward and keep the back of the tongue from blocking the airway.
- CPAP: Short for continuous positive airway pressure, a device, now familiar to most people. The apparatus consists of a mask that goes over the face and is connected to a tube attached to a machine that delivers constant pressure to keep your child’s airway open all night, ensuring adequate and consistent breaths are taken. Of course, since children grow quickly, your child’s CPAP will have to be adjusted and re-fitted at least every six months to ensure efficacy, and it’s only approved for children 7 and older.
-
-
- Dental appliances: Though these will be described in more detail below, dental appliances are another effective, non-invasive way to help treat OSA in children.
-
-
- Tongue/lip-tie release: Many infants and children have lip and/or tongue ties which don’t allow for normal range of motion. These can have profound influences on a person’s inability to breathe through their nose, or in the case of infants, to breastfeed.
- Surgery: Once more common but still widely used, adenotonsillectomy is the surgical removal of the tonsils and adenoids. This surgery has been very helpful to many children, especially those with OSA. The main benefits of Tonsillectomy and Adenoidectomy are: better-quality nocturnal breathing, reduced snoring, decreased enuresis (bedwetting), better behavior, and improved growth.
-
How Dental Appliances Can Help with SDB
Due to the invasiveness of surgery and the discomfort many children experience with a CPAP machine, a wonderful alternative to these SDB therapies is the relatively-new realm of oral (dental) appliances. Just over two decades in existence, functional or orthotropic dental appliances can help children with SDB when used early on. Examples include the Healthy Start, Myobrace, and the Daytime-Nighttime Appliance (DNA). It’s best to meet with your child’s orthodontist to determine what type of appliance will be most appropriate and helpful for their case.
In children, an oral device called a modified monobloc appliance has been shown to significantly help children with OSA over 6 months of therapy or more. Benefits include not only decreased apneic episodes, but also improved sleep quality and daytime performance in children who have used this treatment modality.
vances are wonderful news to parents everywhere; your child has a plethora of ways available to help her breathe and live better. It’s only a matter of getting diagnosed, then treated, so that your child can live up to her full potential.
Your Dentist Can Screen You or Your Child for Sleep Disturbance Problems
The American Dental Association (ADA) says that dentists should be screening patients for sleep apnea and should be the professionals who are creating oral appliances. Now more than ever, dentists have a key role in identifying sleep disordered breathing early and can help make a great impact on many lives. The earlier SDB is caught, particularly in children, the better the long-term outcome they will have! Be sure to ask your dentist for a sleep apnea screening for you and your child at your next visit.
Do you suspect that your child is experiencing sleep disordered breathing? Get an accurate diagnosis by scheduling an appointment with Dr. Brusky in Green Bay, WI.