Sleep Apnea & Breathing Problems Treatment
You’ve likely heard of the term sleep apnea, as it affects a large portion of the U.S. population. In fact, the American Sleep Association states that 25 million Americans have sleep apnea, with more than ¼ of those aged 30-70 years old suffering from the disorder on a nightly basis.

What is Sleep Apnea?
Sleep apnea refers to times during sleep when breathing completely ceases for 10 seconds or longer, and recurs often throughout the night. There are two main types: the more common obstructive sleep apnea (OSA) and lesser known central sleep apnea (CSA).
If you have OSA, your airway becomes physically blocked, often by muscles that relax too much during sleep. The resulting lack of oxygen eventually causes your brain to wake you up so that you can breathe again.
In the less-common CSA, your brain (not an obstruction) is the cause of the apneic periods. CSA is the result of a miscommunication between the brain and breathing muscles, and is often associated with another problem, like opioid medication side-effects, Parkinson’s Disease, or stroke. Finally, there is also mixed sleep apnea, which is a combination of OSA and CSA.
What’s So Bad about Sleep Apnea?
If sleep apnea is so common, what’s the big deal? Surely people do just fine with it, right? Unfortunately, it can open you up to a whole host of problems, especially the longer it goes undiagnosed or untreated. Since about 80% of OSA goes undiagnosed, it’s important to realize the health impact it can have on you or a loved one.
When you are repeatedly awakened during the night, this has several major impacts on the body. First, it obviously disrupts the sleep cycle. Without adequate amounts of time in each stage of sleep, your body can’t heal and restore itself properly. Over time, this takes its toll physically and mentally. Furthermore, when your body wakes up due to low oxygenation, this causes more secretion of cortisol. Cortisol is a stress hormone given off by increased levels of stress, and over time can harm your vascular system and interfere with how your body processes sugar.
Untreated sleep apnea can put you at risk for the following health problems:
- Asthma
- Atrial fibrillation, a type of dysrhythmia where the atria in your heart beat erratically. This can put you at risk for other problems, like strokes and heart failure.
- Behavioral and cognitive disorders, especially in children. This can include ADD, ADHD, learning disabilities, irritability, and decreased attention, motor skills, and concentration. In older adults, the risk for dementia increases.
- Chronic kidney disease
- Eye disorders, like glaucoma or dry eye
- Fatigue, particularly daytime drowsiness, which can put you at risk for the very fatal drowsy driving, now comparable in mortality to drunk driving. Daytime drowsiness can also put you at risk for a work-related accident.
- Gastroesophageal reflux disease (GERD) and/or acid reflux
- Heart and blood vessel disease, like atherosclerosis, heart attacks, heart failure, high blood pressure, impotence, and stroke.
- Metabolic problems like type 2 diabetes mellitus or insulin intolerance
- Pregnancy difficulties, like gestational diabetes, low birth weight babies, or gestational hypertension
Symptoms that Might Indicate Sleep Apnea
With all these problems associated with this disorder, it’s important that you are aware of what symptoms to watch out for. Oftentimes, it’s a bed partner who will notice these first, as the partner will be, as the name suggests, sleeping.
Some symptoms of sleep apnea include:
- Acid Reflux/GERD
- ADD/ADHD
- Bruxism, also called teeth grinding
- Chronic and loud snoring, one of the most common and prevalent symptoms
- Chronic fatigue and daytime sleepiness
- Depression and/or mood swings
- Difficulty concentrating
- Frequently waking during the night
- Frequent need to urinate in the night
- Headaches or migraines, particularly upon waking
- Impaired memory or judgment
- Impotence or decreased libido
- Irritability
- Scratchy, dry, or red throat upon waking
- Sleep that fails to refresh
- Small jaw
- Tongue with scalloped edges
- Weight gain or obesity
As you can see, a lot of the symptoms are similar to the complications associated with sleep apnea. This may be because this disorder has been going on for some time, and some of the complications are already present.
Risk Factors Associated with Sleep Apnea
Recognizing the symptoms of this condition is important, but so too is knowing what can predispose you to the sleeping disorder, as well. There are several significant risk factors for the development of sleep apnea, particularly OSA:
- Age: Those aged 40 to 70 years old have a higher risk of developing OSA.
- Anatomy: Having a small upper or lower jaw, larger overbite, recessed chin, or large neck diameter (17 inches or greater for men, and 16 inches or greater for women) can put you at a higher risk of OSA.
Commercial motor vehicle (CMV) drivers: CMV drivers have a higher prevalence of OSA than the general population. This is likely due to many CMV drivers being middle-aged males who are overweight. In fact, this is such a risk that CMV drivers are frequently studied when it comes to road safety and sleep apnea.
- Gender: Males are more likely to experience OSA than women.
- Genetics: A family history of OSA can predispose you to it.
- Obesity: Those with a body mass index (BMI) of 35 kg/m² are at a higher risk.
- Post-menopausal women: Those who are not taking hormone replacement therapy (HRT) are at an increased risk of developing OSA.
- Pre-operative patients: Those awaiting bariatric surgery have a higher risk of OSA.
- Substance use: Alcohol, tobacco use, and opioid painkillers can all increase your risk of OSA.
Sleep Apnea is Not the Only Sleep-Related Ailment
While sleep apnea is a serious problem, particularly long-term, it’s not the only disorder that can affect your sleep and your health. Even if you don’t have it, there are other conditions that might put you at risk for health problems. Below are some terms associated with sleep-related disorders.
7 Sleep Issues That Can Negatively Affect Your Health
-
- Hypopnea: Also called “apnea light,” the term hypopnea comes from the Greek roots hypo-, meaning under, and -pnoe, meaning breathing. Thus, hypopnea literally means “under-breathing.” Technically, it refers to a decrease in airflow greater than 50%, with an oxygen desaturation of greater than 3%, or a decrease greater than 30% with desaturation of greater than 4%. This means while you’re not apneic (meaning a 90% or greater reduction of airflow, plus cessation of breathing for 10 seconds), you’re still experiencing periods of under-oxygenation.
-
- Arousal: This is when your body wakes up due to hypoxia (low oxygenation). Traditionally, sleep-disordered breathing (SDB) models tend to follow the path of obstruction to desaturation (hypoxia) to arousal to breathing. Arousal gives us the stimulus to breathe when we’re not getting adequate oxygen. This, however, is the opposite drive to breathing that we normally experience. It’s actually the elevated levels of carbon dioxide (called hypercapnia) that usually drive us to breathe, not hypoxia. Significant periods of arousal typically last three to fifteen seconds.
-
- Apnea-Hypopnea Index (AHI): AHI is simply the number of apnea or hypopnea events per hour. A mild AHI is 5-14.9, moderate is 15-29.9, and severe is greater than 30. This is not a perfect measure, however, and can be altered by modifiers such as the percentage of desaturation and length of each event.
-
- Inspiratory Flow Limitation (IFL): To better understand IFL, try this simple experiment: Take slow, deep breaths in and out through your nose for a full minute. Check your pulse and notice your comfort level. Then, for the next minute, take slow breaths, but stop halfway through the inhalation and hold it for the length of time you’d normally continue inhaling. Then exhale. Do this for a full minute, never taking a complete breath in. Note your heart rate and feeling afterward. You’ll likely notice that your pulse increased, and so did your discomfort! If you’re experiencing IFL throughout the night, imagine how much stress this puts on your body. You’re creating more work of breathing, and giving yourself an arousal response all night long. As you might imagine, this is incredibly taxing on the body and can add to the fatigue already experienced by other sleep problems. IFL can lead to hypertension, adrenal fatigue, tension headaches or migraines, anxiety disorders, and many more problems over time.
-
- Respiratory Effort Related Arousal (RERA): RERA can be measured in sleep studies, and refers to an obstructive airflow reduction. RERA doesn’t meet the definition of either apnea or hypopnea, and is associated with increased respiratory effort that resolves with arousals. Usually, the arousal episodes last more than 10 seconds, and can also be exhausting if experienced throughout the night.
-
- Upper Airway Resistance Syndrome (UARS)UARS is classified by an AHI less than five, an oxygen saturation of greater than 92%, RERAs for more than five hours, all in addition to a feeling of fatigue. If you don’t get diagnosed with OSA, it’s quite possible that you still have a condition like UARS.
- Respiratory Disturbance Index (RDI): RDI refers to a combination of AHI and RERA, or big and little events together throughout the night. This means that your respiration is impacting your sleep, even if it’s not OSA that’s causing the disturbance.
While these terms might seem daunting at first, you can meet with a healthcare professional, particularly one trained in sleep health, to review them with you.
The Severity of Sleep Disturbance: Understanding the Respiratory Disturbance Index (RDI)
More and more, the role of dentistry is heading to the forefront when it comes to detecting sleep disturbances like sleep apnea and upper airway resistance syndrome. Dentists now have an important role in helping facilitate the early diagnosis of sleep disorders, and can help you prevent further health problems down the line.
The American Dental Association issued a news release, dictating the role dentists should play in sleep-disordered breathing. It’s recommended that dentists now do the following:
-
- Assess patients for sleep disorders: Dentists can take note of anatomical abnormalities that can affect breathing during sleep. This can include a large neck diameter, significant overbite, small jaws, recessed chin, and more. Your dentist can complete a thorough evaluation of your upper airway during your next exam.
-
- Evaluate the use of oral appliance therapy: From stabilizing splints to monoblocks (dual arch ARS), to mandibular advancement appliances (MAAs), there are many dental appliances available to help OSA patients. Your dentist can see if your appliance is helping or hindering your quality of sleep.
-
- Identify side effects of oral appliance therapy: If your oral appliance is creating unwanted side effects, your dentist can help you identify a more suitable treatment.
- Communication: As part of a multidisciplinary team, your dentist can relay your treatment progress to ENT physicians and other professionals, like dieticians, oral surgeons, orthodontists, myofunctional therapists, and more.
Sleep Apnea and Treatment Options
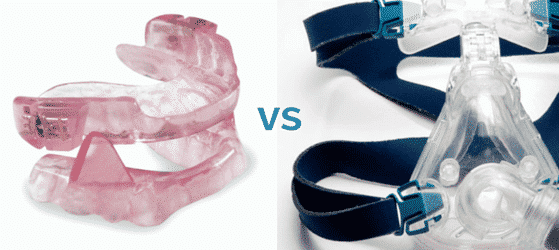
Likely, you’ve heard of the CPAP (continuous positive air pressure) machine, particularly if you’re familiar with sleep apnea. While the CPAP remains one of the best treatments for OSA, it’s not the only one.
Some of the many treatment options include:
- Dental appliances: These often reposition the lower jaw and tongue, making occlusion less likely during sleep. Common apparatuses include mouth guards and splints. Mandibular repositioning mouthpieces and tongue retaining devices are also commonly used.
- Orthodontics: Expanding the palate, helping guide the upper and lower jaws to grow forward, and aligning teeth are some of the best ways to treat the underlying problem of small airways.
- Lingual Frenectomy: Releasing a tied tongue can make a tremendous difference in one’s ability to start breathing through their nose and learning to swallow properly.
-
- Orofacial myofunctional therapy: These therapies are simple and non-invasive, and are helpful at strengthening muscles that control the lips, tongue, soft palate, face, and lateral pharyngeal wall. This can make breathing much easier throughout the night.
- Upper airway surgery (UPPP): This removes tissue in the airway that tends to block it during the night.
- Tonsillectomy and Adenoidectomy: While preferably done before age 7 and in conjunction with myofunctional therapy, even adults may need this to expand airway space and promote nasal breathing.
-
- Nasal Surgery by an ENT: Many conditions of the nasal passages exist which can thwart correct nasal breathing: Stenosis, deviated septum, enlarged turbinates, nasal polyps, etc. By fixing these anatomic problems, proper nasal breathing can be restored.
-
- Hypoglossal nerve stimulation: A stimulator is implanted in your chest, with connections to the hypoglossal nerve and a breathing sensor. The hypoglossal nerve controls tongue movement and helps you get a better night’s sleep by keeping your airway open.
- Treating underlying conditions: Weight loss and smoking cessation programs cannot only resolve your sleep disorders, but can give you a greater quality of life overall.
Have You or a Loved One Been Tested for Sleep Apnea? Ask Your Dentist!
While it’s clear that sleep apnea and other disorders can drastically impact your quality of life, the good news is it’s treatable! The earlier you get diagnosed, the better. Luckily, your dentist can now be a member of your front-line defense against sleep disorders.
Want to know if you suffer from sleep apnea? Be sure to ask at your next dental exam with Green Bay’s Dr. Brusky so you can be evaluated for sleep apnea or other similar problems.