There are many mysteries surrounding the aspect of our lives referred to as sleep. For instance, despite countless studies and armies of experts, the overall why of sleep still eludes us in many ways.
What we do know is that, as human beings, we spend up to a fourth or a full third of our lives sleeping.
We also know that getting a quality amount of sleep has been shown to positively affect our lives in a variety of ways, including the body’s ability to heal, memory and mood, and overall daily function. It’s a chance for us to restore mind and body alike, yet there is always more to learn.
For starters, quality sleep isn’t so much characterized as how much you sleep as how well.
According to The National Sleep Foundation, quality sleep means that you fall asleep within 30 minutes and, more importantly, that you remain sleeping throughout the night with no more than a single awakening. If you do manage to wake up, you drift back asleep within 20 minutes or less.
Bad Sleep is Similar to Being Drunk
We’ve all experienced the opposite of quality sleep, where you’re tossing and turning or staring up at the ceiling waiting for sleep to take you.
It’s that lack of quality sleep that can wreak havoc on the body and our daily lives. In fact, studies show that the more sleep you lack, the more your behaviors begin to mimic someone with a high blood alcohol content.
This is part of what makes sleep so crucial to our well-being. But what happens when we sleep?
The Process of Sleeping Itself
During a night of sleeping for 8 hours, we typically have several 90-110-minute cycles. Initially, the phases go from non-REM stages of transition (stage 1), light sleep (stage 2), and deep or delta-wave sleep (stage 3). These non-REM phases alternate with REM, or rapid-eye movement, cycles. These REM stages account for 25% of our total sleep time, and are when we experience the majority of our dreams. During this time, memory is consolidated and the lessons we’ve learned are cemented in our synapses.
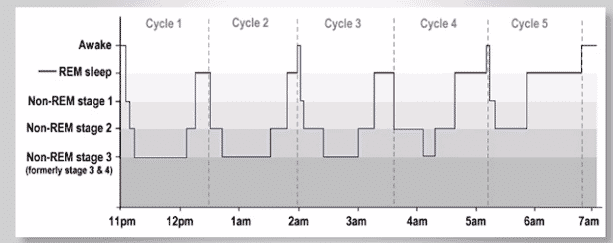
On a given night when you’re falling asleep, your body enters the transition phase, which is generally fairly fast. You then likely go to the non-REM stages 1, 2, and 3, then back up, then to REM sleep. This cycle typically repeats four to six times throughout the night.
Stage 2 of sleep, otherwise referred to as light sleep, accounts for roughly half (50-60%) of our total sleep time. But it’s stage 3 sleep where the most critical aspects of sleep take place. During stage 3, your body is resting and repairing itself. This is otherwise referred to as restorative, slow-wave, or delta-wave sleep. This time period is responsible for our vigilance and general alertness upon waking. It’s also when important functions like muscular pain management, hormone release, and overall physical recovery occur. In fact, stage 3 sleep is so tied to our health and well-being that children really require two to four times the amount of this non-REM sleep than adults do.
If you are constantly waking or can’t sleep and your stage 3 level of sleep suffers, you can begin to develop feelings of paranoia, irritability, mood swings, and general psychological instability. Overall, getting enough of both REM and non-REM sleep is important if you hope to wake up with a sense of well-being.
Sleep Disordered Breathing
One aspect of our lives that can cause disruption in our sleep patterns is what is referred to as sleep disordered breathing or SDB.
The American Dental Association (ADA) characterizes SDBs as potentially serious medical conditions caused by anatomical airway collapse and altered respiratory control mechanisms.
Understanding the Relationship Between Dentistry and Sleep Disordered Breathing (SDB)
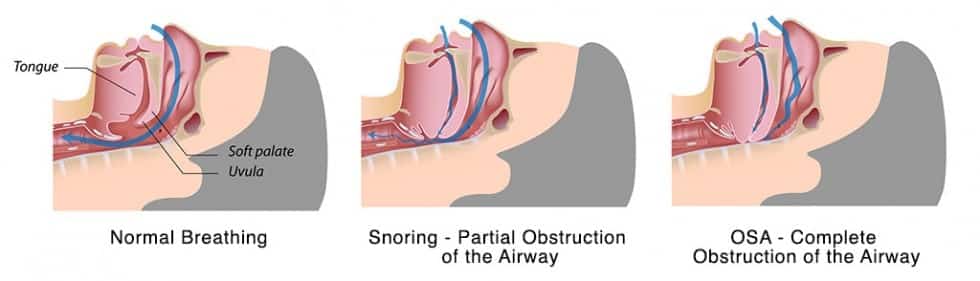
REM sleep is deeply connected to our airways. When we fall into REM sleep, our body temperature drops, blood flow slows, and we have a decreased response to carbon dioxide (CO₂), which drives us to breathe in the first place. As such, when our bodies go into a REM cycle, they decrease the diameter of the upper airway while at the same time increasing our heart rate.
The result, for some individuals with genetically smaller airways, is an increase in pharyngeal obstruction and alveolar hypoventilation. This anatomical alteration makes it significantly harder to breathe throughout the evening, and can drastically reduce the quality of life for those experiencing it. These anomalies are associated with OSA, or obstructive sleep apnea, and affect each year.
What is Obstructive Sleep Apnea?
Obstructive sleep apnea is the most common form of sleep apnea, which causes the body to continuously start and stop breathing through the night.
There are several types of sleep apnea, but obstructive sleep apnea causes the throat muscles to intermittently relax during sleep, which can effectively block your airway.
FUN FACT: The size of your airway is determined in large part by genetics. That means that if your relatives suffer from sleep apnea, you may also.
The National Dental Sleep Foundation estimates that over 80% of OSA sufferers are never diagnosed, but there are signs that can indicate OSA is at work. Learning these signs and symptoms can help you recognize if you or a loved one might be suffering from OSA.
The Signs of Sleep Disordered Breathing
Snoring: One of the first signs of sleep-disordered breathing is snoring: a sign that your airway is constricted or otherwise blocked, which can lead to lack of sleep, poor quality sleep, and subsequent issues.
Sleepiness: If you are excessively tired during the day, despite the fact that you feel you got enough sleep the night before, that could be a sign that you suffer from OSA.
Bruxism: Between 15 and 40% of us grind our teeth while asleep. Teeth grinding, otherwise referred to as bruxism, has been associated with stress and anxiety. However, there is mounting evidence that the grinding of teeth is actually the body’s way of helping itself breathe when airflow is being limited.
You don’t have to be a dental expert to understand that grinding your teeth isn’t good for your oral health. Teeth grinding can lead to excessive teeth wear, fractures, and loosening, which are problems in and of themselves. However, bruxism can also affect more than merely your teeth.
If left to exacerbate, bruxism can affect your chewing muscles and jaw joints. In some patients, their facial expressions may begin to alter to some degree, changing their entire appearance!
Dental Erosion: A huge percentage of patients present with acid erosion on their teeth which can be intimately related to SDB.
TMJ (TMD): Between 70 and 90% of all TMJ sufferers have SDB as a root cause of their condition.
The Dangers of Undiagnosed OSA
We all know the dangers of drinking and driving, but did you know that drowsy drivers can be just as hazardous as drunk drivers? In fact, the National Highway Traffic Safety Administration estimates that caused 90,000 motor vehicle crashes in 2015 alone, with hundreds of fatalities being the result. OSA frequently leads to chronic fatigue, so it’s clear that if you have OSA, you might just be one of those dangerous drowsy drivers.
OSA can also exacerbate diabetes and high blood pressure, not to mention shorten your overall lifespan for these reasons. And due to repeated apneas throughout the night, you’ll be placing undue stress on the heart, which can lead to a heart attack or stroke. Add to this the fact that chronic daytime fatigue can lead to workplace injury, and hopefully you can see that undiagnosed OSA also has an economic burden of $150 billion per year in the US alone!
Symptoms that Might Indicate Sleep Apnea
Aside from snoring, teeth wear, and other obvious signs, here is a list of all the issues that might indicate you suffer from sleep apnea.
- You experience excessive daytime sleepiness.
- You’re fatigued all the time!
- You find yourself frequently waking up during the night.
- Despite getting enough sleep, you never feel fully refreshed.
- You experience impaired memory and judgement.
- You have difficulty concentrating for any length of time.
- You frequently experience depression, anxiety, and/or mood swings.
- You have no sex drive and suffer from impotence.
- Your throat feels scratchy or dry upon waking.
- You’ve been diagnosed with ADD or ADHD.
- You’re a sufferer of acid reflux or GERD.>
- You have frequent and unexplained headaches or migraines.
- You’re irritable and catch yourself grinding your teeth when awake.
Other signs include having a small jaw, tongue with scalloped edges, and redness in the throat. To see if these latter signs apply to you, contact your dentist for an evaluation of your oral anatomy.
Treatments for Sleep Disordered Breathing
CPAP Machine: A continuous positive airway pressure (CPAP) machine has traditionally been one of the most common and effective treatments for sleep apnea. The machine is designed to help people with sleep apnea breathe easier and more regularly while sleeping.
The technology uses a filter and small tank of water that works as a humidifier. A mask or nasal “pillows” connected to a tube is placed over your face or nostrils while you sleep and a chin strap holds the apparatus in place. There are some CPAP machines that do not use straps.
When turned on, the CPAP machine works by increasing the air pressure in your throat. This prevents your airway from collapsing when you inhale, and making sure that you have no periods of sleep apnea throughout the night.
The machine has an added benefit of decreasing snoring, which is great news for anyone who sleeps beside a person with sleep apnea.
There are variations to the CPAP machine. Some come with masks that cover your nose and mouth while other masks cover only your nose. The latter is known as a nasal continuous positive airway pressure machine or NCPAP.
If wearing a mask attached to a machine makes you wary, you’ll be glad to know that there are a range of benefits from using the CPAP machine, other than helping you sleep better.
- You’ll feel less fatigued during the day
- You will experience far more energy compared to life before using the CPAP
- You might notice that you snore less or not at all
- You may find yourself dropping some pesky pounds! That’s right, the CPAP has even been linked to weight loss.
How a Dental Appliance Helps with Sleep Disordered Breathing
One downside of the CPAP machine is that many patients don’t comply with its use over time. Though studies vary in their numbers, about 50% of CPAP users will eventually abandon their machines within a year or two. This percentage increases if patients have to wear their CPAP more than 4 hours at night. Some report not liking the noise created by the machine, the hassle of keeping the mask affixed for so many hours, or the effect it has on their relationship with their bed partner.
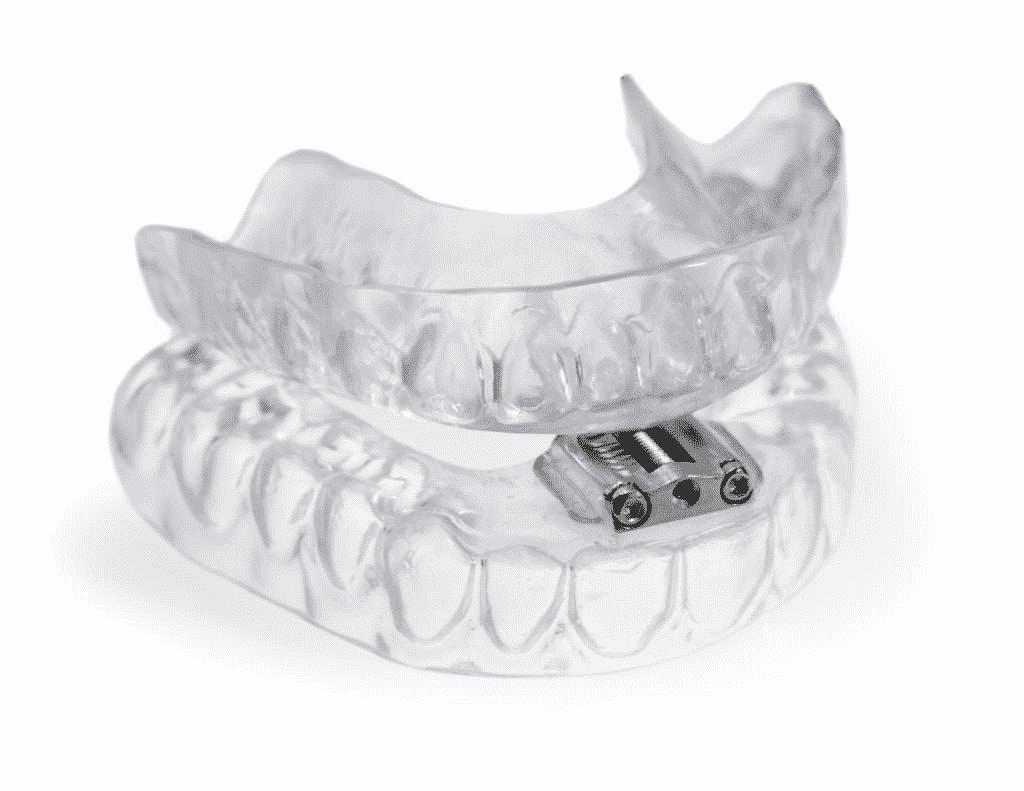
Luckily, there are dental alternatives to the CPAP that are equally effective! The most commonly-used oral appliance is called a mandibular advancement appliance (MAA), which is a customized device that is fitted exactly to your mouth. The goal of an MAA is to prevent your mouth’s soft tissue from collapsing into your airway, which disrupts breathing and can lead to sleep apnea. MAAs are also used to prevent snoring, and are preferable to many patients when compared to a CPAP.
The MAA is typically worn on both upper and lower teeth and is adjusted by your dentist to make sure your airway stays open when you sleep. It’s a great, non-invasive alternative to surgery, which is another method of treating sleep apnea. Additionally, your bed partner may prefer this treatment, since it is silent, unlike the often loud CPAP machine. There are many variations of the basic MAA design, so you can work with your dentist to find the right fit for you!
How Will Your Dentist Test for Sleep Disturbance?
When you visit your dentist for your semi-annual checkup, he might ask some questions to see if you are experiencing any sleep disturbances. If he suspects SDB, you and your bed partner may be asked to fill out some sleep questionnaires, which then may prompt a Home Sleep Study with a monitor to be performed. These inquiries can help prevent any serious problems in the future, and are key to your overall health.
Common questions include:
- Do you snore loudly?
- Do you often feel tired or fatigued during the day?
- Has anyone observed you breathing less or not breathing while asleep?
- Are you or have you ever been treated for high blood pressure?
- Do you have restless sleep?
Working together with your dentist, you can ensure that you’re taking necessary steps to dealing with any potential breathing complication you may have. By early screening and interventions, you won’t have to worry about untreated, undiagnosed OSA; you’re already taking care of it!
Putting It All Together
In summary, sleep is essential to our physical and emotional well-being. It’s crucial to a good quality of life, and is a need we face on a daily basis. When sleep is interrupted, this deprivation can wreak havoc on body and mind alike, so early intervention is key. Luckily, new advances in dentistry and sleep science make it possible to detect sleep disordered breathing sooner rather than later and potentially treat more mild cases before they progress to full blown sleep apnea.
Be sure to get regularly screened and assessed by your Green Bay Dentist, Dr. David Brusky. With sleep and dentistry so intrinsically linked, you owe it to yourself to get checked for sleep-disordered breathing and other problems that may be preventing you from living a full and healthy life.
Schedule your next appointment with Dr. Brusky right now in Green Bay, WI.





 source
source